Screening process ensures meds are used most effectively.
A recently developed screening process that detects a mutated form of Hepatitis C virus (HCV) is helping ensure that a costly HCV medication is prescribed only to patients who will benefit from it.
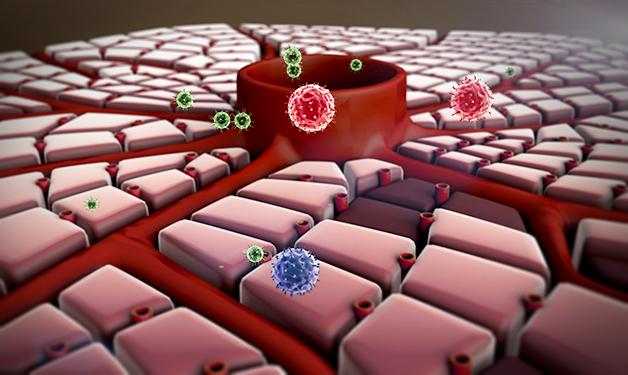
Hepatitis C is a chronic blood-borne liver disease that affects an estimated 242,500 individuals in Canada1.
Tailoring treatment will mean cost savings and the potential of eliminating the virus altogether.
A fairly new drug named simeprevir is a potentially highly effective treatment for HCV. However, when simeprevir is used in combination with other drugs (interferon and ribavirin) in HCV patients carrying a specific type of virus polymorphism, called “Q80K”, its efficacy is reduced. As a result, the U.S. FDA and Health Canada made it a recommendation that patients starting this therapy be pre-screened for the HCV Q80K variant. This helped launch the development of a screening process in Canada.
Vancouver Coastal Health Research Institute-affiliated researcher Dr. Richard Harrigan, Director of the Laboratory Program at the B.C. Centre for Excellence in HIV/AIDS (BC-CfE) and Professor in the UBC Faculty of Medicine, led the development of the screening process in partnership with Janssen Inc., the manufacturer of simeprevir, the BC Center for Disease Control, and funder Genome BC.
“We did a lot of research into a number of things: the best technical ways of amplifying and sequencing the virus, how this mutation came about in the first place from an evolutionary sense, and how it spread around the world,” says Dr. Harrigan. “We discovered that the mutation probably popped up in the U.S. many decades ago.”

“Screening for the Q80K mutation prior to prescribing simeprevir helps doctors tailor treatments according to the needs of each individual HCV patient,” says Dr. Harrigan. “This is important not only for reducing unnecessary treatment costs, it could also lead to a dramatic reduction in the spread of HCV.”
Based on 2007 national estimates, that year an estimated 802 Canadians developed cirrhosis, 473 progressed to liver failure, 292 had liver cancer, and 134 received a liver transplant due to HCV.
“By applying a similar approach that has already proven successful in managing HIV and AIDS, specifically tailoring treatments to match individuals, we have the best chance of eliminating the HCV virus,” Dr. Harrigan says.
“These newer therapies are completely changing the landscape of Hepatitis C treatment.”


