
A family clustering protocol for relatives of patients with early-onset cardiovascular disease boosted proactive care initiation.
An early screening and treatment approach examined in a study led by Vancouver Coastal Health Research Institute researcher Dr. Liam Brunham enhanced preventative treatment interventions for the first-degree relatives of patients with premature cardiovascular disease.
“We know that heart disease can have a very strong genetic component when it occurs at an early age, and that early interventions such as medications and lifestyle changes are key preventative strategies,” says Brunham. “Our family clustering approach identified relatives with cardiovascular risk factors or evidence of cholesterol build-up in their blood vessels. Many of these relatives were unaware of the severity of their risk and were not taking medications that could aid in disease prevention.”

Heart disease, also known as cardiovascular, coronary or ischemic heart disease, impacts around one in 12 Canadians aged 20 and older. The second leading cause of death in the country after cancer, the condition has recently been on the rise among young adult British Columbians.
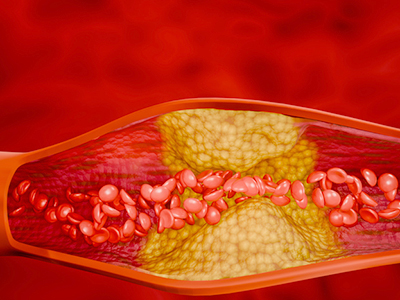
If left untreated, this chronic condition can lead to serious and potentially fatal consequences, such as heart attack, heart failure and death. Stroke can also occur when plaque forms in the blood vessels to the brain.
Imaging could enhance patient diagnostics and treatment adherence
Brunham’s study, published in the American Journal of Preventative Cardiology, recruited 132 immediate family members of patients with premature cardiovascular disease who participated in the longitudinal Study to Avoid cardioVascular Events in British Columbia (SAVE BC).

“While screening the first-degree relatives of patients with premature coronary artery disease is recommended, it is not commonly performed in clinical practice,” Brunham notes.
"The prevalence of significant early-stage atherosclerosis is far higher among patients with a family history of premature cardiovascular disease than it is in the general population.”
The research team diagnosed around 34 per cent of participants with early evidence of atherosclerosis, most of whom were identified as having moderate to high cardiovascular disease risk. Some of the heart disease risk factors were abnormal lipid levels in the bloodstream among 37 per cent of participants, obesity among 25 per cent and high blood pressure among around 22 per cent.
Approximately 33 per cent of participants were placed on a lipid-lowering medication, with another 16 per cent recommended to intensify their lipid-lowering therapy.
Notably, about 83 percent of study participants who had imaging of plaque in their arteries during the study followed through with the recommended lipid-lowering therapy, compared with only 45.5 per cent of participants who did not have imaging evidence of plaque.
“Seeing is believing. Imaging is a powerful tool, and makes these important risk factors more tangible and real for our patients, which we know can help optimize adherence to medical recommendations.”
“We found that patients with a family history of premature cardiovascular disease and with low or moderate risk of cardiovascular disease would benefit from the type of family-based screening performed in SAVE BC,” says Brunham. “Showing patients the coronary arterial plaque buildup in their diagnostic images may improve their uptake of preventive medications.”
Brunham and his team are presently investigating a new early warning clinical assessment tool that would also consider genetic risk scores of heart disease.
“We have established evidence for an early cardiovascular disease screening tool based on first-degree relatives, but more research is needed to further validate this approach and to understand the nature of risk in these patients that is not accounted for by traditional cardiovascular risk factors,” states Brunham.


