
A novel, eight-step approach tested in a critical care setting lessened negative feelings and moral conflict that can lead to burnout.
Going against one’s moral compass can generate a sick feeling in the stomach. It is also a contributing factor to the emotional distress that is pushing some health care workers out of the profession.
A research study led by Vancouver Coastal Health Research Institute researcher Dr. Peter Dodek investigated the effectiveness of a novel approach to help reduce moral distress among health care workers at a Vancouver-based, 11-bed intensive care unit (ICU).

Moral distress is often experienced in situations such as end-of-life care, communicating with patients’ family members or differences of opinion on how to proceed with treatment. It can be characterized by feelings of anger, powerlessness and guilt, explains Dodek.
Having lived through his own bouts of moral distress as an ICU physician, Dodek understands why moral distress can also diminish workplace satisfaction and lead to absenteeism, burnout and attrition.

Finding new approaches to reduce burnout and retain nurses is essential given current health care staffing shortages and the fact that it costs around $100,000 to fully train an ICU nurse, says Dodek.
Moral Conflict Assessment tool reduced distress in eight steps
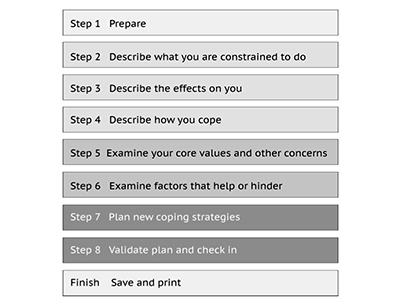
Dodek’s study, published in the Canadian Journal of Anesthesia, discovered that an eight-step process empowered health care workers and reduced their feelings of moral distress.
The novel Moral Conflict Assessment (MCA) tool used by the research team built on concepts found within participatory action research, engaging both researchers and participants in a process that involves self-reflection and moving understanding into action.
Six bedside ICU nurses and two ICU allied health professionals were guided through the steps over the course of three 1- to 1.5-hour sessions. Participants identified a moral conflict situation that involved an end-of-life patient in his mid-60s who received critical care in the ICU. Aggressive life-support and intermittent cardiopulmonary resuscitation had been provided to the unconscious and near-death patient.
“The situation led to a high degree of collective stress,” notes Dodek. “Some participants shared that they experienced feelings of discouragement, fatigue, helplessness, apathy and frustration. The aggressive treatment intervention made some feel sorry for the patient and shame for potentially going against his wishes.”
These feelings led to sleep disturbances and withdrawal from work. To cope, some participants turned to exercise, listening to music or taking medication to aid with their sleep.
Working through the MCA process, participants reached a consensus on four recommendations to address gaps in the provision of care, improve communication chains and reduce moral distress in the ICU:
- Clarify which physician is responsible for the care of patients who have come from other wards to the ICU to receive intermediate care;
- Create a clear and consistent care plan for each patient that is shared with other care providers, as well as the patient’s family;
- Assign trusted communicators to provide coordinated and consistent care to the family members of seriously ill patients; and
- Enhance trust and understanding by educating family members of ICU patients on advance care plans and the nature of death and dying, as well as by educating ICU clinicians on forms, legal liabilities and ethical considerations.
At the end of the study, all four recommendations were implemented in the ICU.
“Participants saw this process as a vehicle to express themselves and hopefully engage with decision-makers about how to minimize moral distress,” says Dodek. “The solutions participants identified were realistic and did not require additional funding or staff positions.”
The MCA tool has been used at several hospitals to-date. Dodek says that he and his team plan to continue assessing its potential applications and outcomes in health care settings in future studies.
Learn more about the free, eight-step Online Moral Conflict Assessment tool.


