
Researchers delve into uncharted territory, gathering data to help understand the care needs of people with severe concurrent disorders.
A breakthrough study of individuals in Greater Vancouver receiving treatment for substance use and mental health disorders identified significant unique characteristics among cannabis users and non-users. Led by Vancouver Coastal Health Research Institute researcher Dr. Christian Schütz and Karina Thiessen, the first-of-its-kind study found a disconnect between study participants and the general public, underscoring the importance of research inclusive of populations that are often unreached.

“The relationship between cannabis use and mental health continues to be widely debated in the scientific community and among the general public,” says Schütz. “Our study contributes to this discussion by examining health outcomes of vulnerable individuals with severe and comorbid mental health and substance use disorders who are often excluded from studies.”
“In particular, there is a lack of cannabis research on vulnerable populations in regions where recreational cannabis has been legalized.”
Prior research has found associations between cannabis use and an increased risk of adverse mental health outcomes, including anxiety, depression and psychosis, particularly among younger individuals, says Schütz. “People with psychiatric disorders have been found to have higher rates of cannabis use compared to the general population. They are also more likely to use high-potency cannabis that has become more available in recent years.”
Unique self-reported symptoms in need of further investigation
Schütz and Thiessen’s study involved 211 individuals who had received at least one month of treatment at the Red Fish Healing Centre (RFHC) — a tertiary integrated treatment facility in Coquitlam, B.C. — with 100 participants reporting no recent cannabis use and 111 reporting cannabis use at least once every 30 days. RFHC offers physical therapy, social work services, recreational activities and medical and group therapy for individuals with concurrent disorders who have exhausted other available treatment options.
The study team compared data from participants that were in treatment before recreational cannabis was legalized in Canada in 2018 with individuals who were in treatment after legalization.

Medical charts provided information on participant admission dates to RFHC and diagnoses at admission. Participants completed a survey that included a clinical cannabis use questionnaire and the Symptom Checklist-90-Revised, a standardized questionnaire to evaluate symptoms of mental illness and psychological distress.
“We noted differences between self-reported symptoms and diagnoses — which can have overlapping symptoms — pointing to the need for a nuanced and comprehensive perspective of mental illness to capture patients’ experiences,” Thiessen shares.
Study participants who used cannabis tended to be younger, to be male, to use more types of substances and to have higher self-reported depression, anxiety and psychotic symptoms. Male participants were also more likely to be diagnosed with mood disorders. “This is the opposite of what we see in the general population and may reflect the severity of mental illness in the male participants included in our study,” says Thiessen.
“Our results indicate that patients who used cannabis may be experiencing more distress overall.”
The distress patients experienced may be due to them potentially using cannabis to cope and self-medicate; potential negative impacts of cannabis use on mental health; or a common factor that increases the likelihood of both cannabis use and mental distress, Thiessen adds.
Among participants who used cannabis, older individuals were more likely to be diagnosed with a mood disorder, such as major depressive disorder or bipolar disorder. However, participants who began using cannabis at a younger age were less likely to self-report psychoticism symptoms, such as difficulties differentiating between reality and false beliefs or feeling disconnected from others.
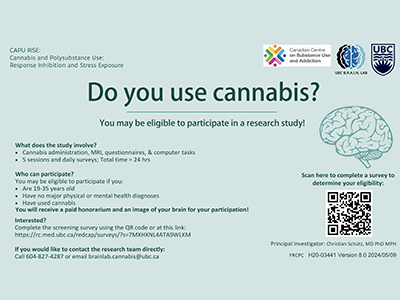
Schütz is currently leading a large, longitudinal, multi-site Reducing Overdose and Relapse: Concurrent Attention to Neuropsychiatric Ailments and Drug Addiction (ROAR CANADA) Project that follows vulnerable individuals with severe concurrent substance use and mental disorders in B.C. and Ontario. Early findings from this study were recently published in the Canadian Journal of Psychiatry.


