
Made-in-BC product promises relief for patients with painful and hard-to-heal wounds.
A new product developed in BC by Vancouver Coastal Health Research Institute (VCHRI) scientist Dr. Aziz Ghahary may solve the painful health burden of slow healing wounds. These wounds include pressure ulcers (or bedsores), large burns, and diabetic sores. They are very costly to treat. In BC alone, the cost of treating pressure ulcers in spinal cord patients is about $50 million per year. Pressure ulcers come from hours spent immobile in wheelchairs or in bed. Circulation becomes cut off, tissue is destroyed, and the resulting wounds are deep and painful. Actor Christopher Reeves (Superman) is reported to have died from pressure ulcers that became infected.
Ghahary’s new MeshFill product could cut stave off wound infection, reduce treatment times (and costly hospital stays) and improve healing outcomes for hard-to-heal wounds. MeshFill is a liquid skin substitute that has performed well in lab testing. Ghahary received a 2017 VCHRI Innovation and Translational award for MeshFill and just received approval to test the product on a group of spinal cord patients at Vancouver General Hospital (VGH). He believes it will be a game-changer.
“When spinal cord patients develop pressure ulcers, it can have significant negative impact on their quality of life. Many can’t go out and socialize or work. Some of them say the ulcers are worse than the paralysis because they are in so much pain and unable to heal. MeshFill may be a cost-effective answer to improve their situation.”

Ghahary says MeshFill works by providing a scaffold to support skin cells while they rebuild and heal. Not only is MeshFill a scaffold, it also acts as a mortar. In the case of pressure ulcers, the product can fill in the void left from destroyed tissue and give new skin grafts something to build onto.
"Deep wound repair is like building a wall. You need mortar to hold the 'bricks' of cells together or else they will collapse. MeshFill acts as that mortar."
In the case of large burns, which are shallower, skin meshed grafts have had more success in closing wounds, but they tend to leave behind a fishnet appearance. Essentially, a large piece of skin is scored with grooves and draped over a wound. Ghahary says this means it’s impossible to have a smooth finish on the final healed wound. He says MeshFill could solve this problem too, and not just for burn patients.
“MeshFill has many potential applications, beyond burns and pressure ulcers. We can apply the product to a range of skin lesions including cavities left after removal of melanomas. And we have also seen tremendous results for diabetic wounds which are notoriously slow to heal.”
Potential to help patients around the world with little risk of infection
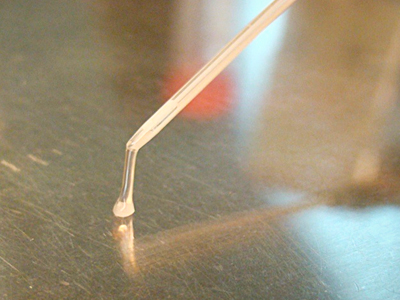
“Although it needs to be applied as a liquid, at a precise temperature, we have engineered the product to be in powder form so it can be easily shipped anywhere in the world, without worrying about temperature control. It can then be reconstituted to a liquid in the operating room where it starts to harden and fill in wound cavities.”
MeshFill is made of natural skin proteins, so Ghahary uses a new electron-beam radiation technique to destroy any bacteria or germs. The resulting substance is classified as a device, not a drug, because it remains at the site of application. It does not enter the blood stream, so there’s very little chance of it being circulated into any other organ and causing a body reaction.
Ghahary is excited to see the results of the VGH trial of MeshFill. He’s grateful to both the VCHRI Innovation and Commercialization awards and the Michael Smith Foundation for Health Research for supporting his work.


