
Near-infrared spectroscopy could make it possible to better treat and prevent muscle control disorders such as spasticity.
Even the most seasoned weightlifters will feel the burn after pumping iron for a few sets. Their muscles cue their brain to take a break and relax, but for spinal cord and brain injury patients, that muscle-brain connection may be damaged or severed. This disconnect can lead to a painful condition called problematic spasticity, when muscles fire involuntarily and relentlessly.
“Around 30 per cent of stroke patients will develop problematic spasticity1, and that number is around 70 per cent for spinal cord injury patients2,” notes Vancouver Coastal Health Research Institute clinician researcher Dr. Patricia Mills. “People with traumatic brain injury, ALS, cerebral palsy and MS, among other conditions, are also at risk of developing problematic spasticity.”

Proven treatments exist to help relax spastic muscles—such as botulinum toxin injections—but a knowledge gap has precluded the development of a quantitative diagnostic test to determine when and how often to administer them.
Mills and colleagues’ study into the use of near-infrared spectroscopy (NIRS) to detect spasticity—recently published in the Journal of the Neurological Sciences, the official journal of the World Federation of Neurology—points to a technological innovation that could help fill the gap.
“The use of NIRS is a new frontier in spasticity diagnostics.”
Their study is one of the first to provide empirical evidence in support of using NIRS (pronounced “nears”) as a qualitative assessment tool for measuring key indicators of spasticity.
Tracking blood flow and oxygenation could help predict and prevent problematic spasticity
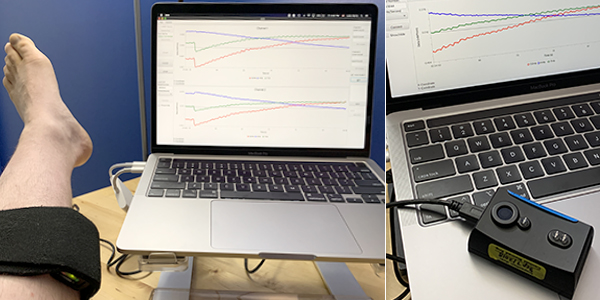
Similar to magnetic resonance imaging (MRI) and electroencephalography (EEG) machines, NIRS technology provides a picture of what is happening inside the body. But unlike those imaging tools, NIRS is often portable and much less expensive.
NIRS emits photons, which are tiny particles that form the basis of light, explains study co-author Dr. R. Luke Harris.
In spasticity research, this non-invasive and non-tissue-damaging invisible light is used to monitor characteristics in blood flow. Specifically, it calculates levels of hemoglobin—the oxygen-carrying protein found inside red blood cells—and oxygen levels in the blood passing through tissues.
"NIRS photons ‘bounce’ around in the tissue, rebounding off of various molecules like balls on a pool table.”
“When photons bounce, their energy changes. We then compare those changes with the photons that were first emitted to identify certain features in the tissue,” says Harris.
NIRS technology takes a snapshot of how much blood is flowing in an area of the body, and how much oxygen is in that blood—similar to how much traffic is on a road and how many passengers are in each car. In healthy individuals, blood flows smoothly through veins and muscles, and has enough oxygen to keep tissues healthy.

In patients with problematic spasticity, blood flow may be restricted or stopped, and there may not be enough oxygen in each blood molecule ‘car’. Over time, this can lead to muscle damage.
Researchers are still unclear about how exactly to use blood flow and oxygenation tracking information to predict the improvement or worsening of spasticity. However, Mills anticipates that NIRS will help gather essential data to develop predictive models to treat and prevent it.
“A more sensitive tool, such as NIRS, could be a better predictor of disease progression, which supports our aim of administering the right treatment at the right time,” remarks Mills.
"We are looking for the ‘Goldilocks zone’ when treatment is administered neither too early nor too late.”
Mills also anticipates that data collected using NIRS could allow researchers to identify trends in different injury types, such as spinal cord and brain injury, to determine when best to provide certain interventions, such as muscle relaxants, to that patient population.
“Our long-term goal is to use NIRS to prevent spasticity through early and patient-tailored treatment interventions,” says Mills.
1 Stroke Foundation - Muscle spasticity after stroke
2 World Journal of Orthopedics - Chronic complications of spinal cord injury


