
Priority access to initial vaccine supplies and protective equipment for the long-term care sector, along with a positive attitude, helped one facility navigate the challenges of COVID-19.
Care providers and people living in long-term care homes were among the most affected by the COVID-19 pandemic. A study led by Vancouver Coastal Health Research Institute (VCHRI) researcher Dr. Lillian Hung explores how the person-centred culture of care and positive attitude at one care home brought staff and residents closer together and improved the mealtime experience for residents.

“A lot of media coverage has focused on the negative impacts of the pandemic on long-term care homes, some of which have been sites of both loss and tragedy,” says Hung. “Our research found that there are also positive stories about care providers and residents coming together that need to be shared.”
Hung’s Happy2Eat practice improvement project, which received a 2019 VCHRI Team Grant, launched a weekly series with staff at the VCH Minoru Residence long-term care facility in Richmond, B.C., which is home to around 250 seniors.

Hung’s qualitative research study builds on the CHOICE+ program developed by Dr. Heather Keller. CHOICE+ makes available educational materials and checklists that use a person-centred care approach, which focuses on addressing individual needs, to improve the mealtime experience and dining environment of people living in long-term care facilities.
“We applied the CHOICE+ evidence-based program to our study to determine whether or not it could help staff improve their care practices,” says Hung. “The approach we took was very participatory, involving team leads and frontline staff, as we knew that we would need to work with staff and understand their experiences.”
Coming together to address pandemic challenges
The project was initially designed to involve in-person meetings when Minoru staff members gather for a ‘huddle’ after lunch and dinner on Fridays. Following the start of the COVID-19 pandemic in March 2020, the project shifted to virtual meetings that focused more on how staff were coping with their work and connecting with the shifting needs of care home residents.
Hung gathered feedback from 29 nurses, care workers and recreation staff, as well as a unit clerk. Questions surrounded how they were able to support residents during mealtimes, what was working well and lessons they learned through their experiences.
“People really had to adapt and adjust. Staff said they were very proud of the work that they do and also felt very anxious,” says Hung, whose research was featured alongside over 2,600 posters and almost 500 presentations at the Alzheimer’s Association International Conference in Denver, Colorado in July 2021.
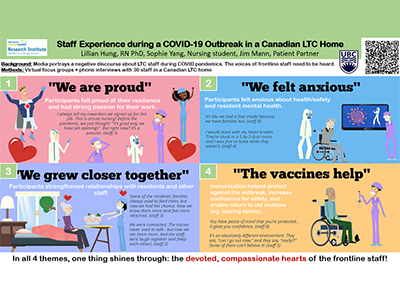
One of four themes revealed through Hung’s research (see the image above), staff anxiety was compounded by feelings of being isolated from family and friends, and experiences with being stigmatized by some community members.
“One staff member shared how when she went to the bank and told a bank teller that she worked in long-term care, he immediately pulled back and washed his hands,” states Hung.
Despite the challenges associated with the pandemic, staff retention at Minoru was quite high. This, Hung says, was likely related to their early access to essential personal protective equipment (PPE) supplies and training, and the fact that they were one of the first facilities to receive vaccines.
Staff’s ability to collaborate and find pride in their work supported them during the pandemic.
“One of the nurses noted that staff had to put aside any differences they may have had, and work together to get things done,” Hung says. “It was interesting to see how they stuck together to do their work, and came up with creative ways to support the residents’ dining experiences during a very difficult time.”
In addition to robust public health guidelines and infection prevention and control practices, to increase staff comfort in the work environment during a COVID-19 outbreak at Minoru, staff asked residents to raise their hand before they coughed, if possible, to give staff time to move back. “Even though nurses wore full PPE, such as a face shield and mask, and practiced excellent hand hygiene, this technique helped give them greater peace of mind.”
Spending more one-on-one time with residents who needed to stay in their rooms for mealtimes also deepened staff’s relationship with them, says Hung. “They told me that they had an opportunity to learn more about residents’ personal stories and get closer to them.”
“Minoru staff members are knowledgeable, skillful and compassionate. They provide commendable person-centred care to residents during their dining experiences.”

Leadership team members listened to staff needs and feedback, which not only helped staff with their daily tasks, such as feeding residents, but also created a more collaborative work environment, says Hung.
As a result of Hung’s research study, Minoru now staggers mealtimes so that they are less rushed. “This makes it easier for everyone to enjoy the mealtime experience.”


