
The pandemic has shone a light on the need for decision-making tools and public input to support health-care resource allocation.
Deciding which patients to treat and when were among the many challenges presented by the COVID-19 pandemic.
With limited resources and staff available to care for patients, health care decision-makers were faced with an unprecedented situation in which patients and health-care resources needed to be allocated based on ever-evolving rules and guidelines.
In his study, Vancouver Coastal Health Research Institute (VCHRI) researcher Dr. Craig Mitton examined how to balance economic and public health priorities following the early and more uncertain stages of the COVID-19 pandemic.

Published in the journal Healthcare Management Forum, Mitton’s study highlights the utility of formal priority-setting tools to aid decision-makers with allocating resources.
In the wake of substantial spending during the first year of the COVID-19 pandemic, the growth of economic debt in Canada and a backlog in care for certain procedures, such as elective surgeries, the approach proposed in his research could clarify the decision-making process and enhance its transparency, Mitton says. The fact that decision-makers chose to preserve hospital capacity by cancelling elective surgeries had real and detrimental impacts on patient well-being and outcomes, he adds.
“Did we make the right trade-offs? Why did we prioritize COVID-19 patients over all others in the system? These are the hard questions we need to ask.”
“As the pandemic progressed — and as we had more information about the virus — decision-makers should have been using a decision-making framework to engage with the public and assess how the values underlying their approach informed decisions surrounding trade-offs,” he says. “Maybe the process would tell us that COVID-19 patients should be prioritized, but maybe not.”
The case for a formal process and public engagement
In the early days of the pandemic, public health officials preserved hospital capacity to make room for COVID-19 patients. As more became known about the virus and how it was transmitted, Mitton’s research suggests that health care decision-makers should have introduced a more formalized process of decision-making, and one that involved greater public input.
In his study, Mitton proposes a formal approach to priority setting and resource allocation that incorporates the Program Budgeting and Marginal Analysis (PBMA) and Accountability for Reasonableness (A4R) frameworks. Both frameworks have been used for many years to assist decision-makers in determining how best to allocate scarce resources.
To further evaluate the relative value of available options, Mitton’s research suggested using Multi-Criteria Decision Analysis (MCDA), which assesses competing criteria, such as cost, risk and resource availability. The approach is useful for determining the most cost-effective course of action to meet the greatest need.
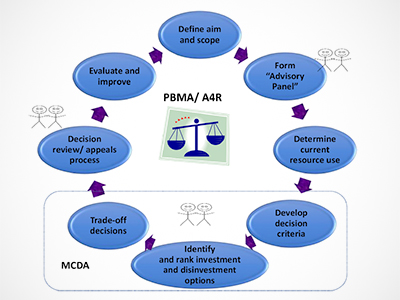
Mitton’s “Process for priority setting and resource allocation in health care” combines the PBMA, A4R and MCDA approaches, and highlights key areas for public involvement throughout the process lifecycle.
Public engagement can not only assist with priority setting, it can also help to inform the response to future pandemics and retain trust in Canada’s public health care system, he says.
“In addition to giving more people a voice in the decision-making process, the process could provide a rationale for the choices made.”
“The approach should involve identifying the priorities, people and underlying values that should inform decision-making,” Mitton says. “Having a framework in place can enhance decision-making and optimize the use of our limited health-care resources.”


