
Widespread efforts to combat COVID-19 have underscored a need for a personalized medicine approach in research.
A greater understanding of how COVID-19 affects people individually has researchers calling for a more targeted and cross-disciplinary approach to medical research and patient care.
“There can be a tendency in the health care field to operate in silos,” says Dr. Mypinder Sekhon, a Vancouver Coastal Health Research Institute (VCHRI) scientist and the lead author of a editorial on the COVID-19 cytokine storm syndrome (CSS) controversy that was published in the European Respiratory Journal.

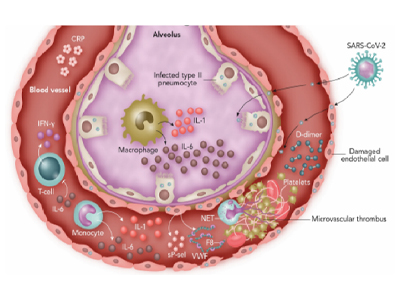
Cytokines are inflammatory signaling molecules that attack infections and other antigens. CSS occurs when the body’s immune system goes into overdrive, causing dangerously high levels of inflammation that damages healthy cells and can lead to organ failure—although, as Sekhon points out in his article, there is no official definition of CSS.
The precursor to Sekhon’s editorial was the challenge clinicians faced when trying to identify which COVID-19 patients were more at risk of developing CSS.
“With COVID-19, there were two camps of thought: one believed that the virus was causing severe illness, while another believed patients’ immune systems were the main culprit, but the answer was that patients have different responses to the virus for various and complex reasons.”
Patient segments revealed a cause of the COVID-19 cytokine storm
Sekhon’s analysis of recent COVID-19 clinical findings highlights that severely ill COVID-19 patients tended to have elevated levels of inflammatory immune system-regulating proteins secreted by the body’s cells. Higher amounts of these mediators in the bloodstream can be an important biomarker of potentially concerning levels of inflammation.
However, while blocking the actions of these inflammatory mediators can help improve some COVID-19 patients’ symptoms or disease severity, there is considerable heterogeneity in patients’ responses to COVID-19, says Sekhon. “This points to why we need to move beyond a one-size-fits all approach to this complex disease.”
“The current approach of many COVID-19 clinical trials has been to include all patients. However, given the drastic differences in the individual responses to this viral infection, we must focus on more targeted approaches.”
Segmenting patients into cohorts based on unique, identifiable characteristics is key, he says.
While around 80 per cent of COVID-19 patients will have mild symptoms, for 20 per cent of patients, infection can be severe, have long-lasting health effects and be potentially deadly. The more care can be tailored to meet the needs of each patient, the better their treatment outcomes are likely to be, says Sekhon.
Sekhon adds that the road to personalized care can often be made sturdier through collaborations between multidisciplinary teams.
“Complex problems, such as COVID-19, require a concerted effort by researchers from various disciplines, departments and areas of expertise,” he says. “A multidisciplinary approach can help us develop a better understanding of a disease and a bench-to-bedside research program.”
“We are all on one team with the common purpose being to care for patients. We need to continue to take advantage of each other’s expertise and learn from one another.”


