Advances in artificial intelligence technology could save patients from unnecessary polyp excisions and lab result wait times.
An innovation in artificial intelligence (AI) technology is aiding clinicians in identifying and classifying polyps and adenomas that could lead to colorectal cancer, according to the findings of Vancouver Coastal Health Research Institute researcher Dr. Michael Byrne.
His review, published in the Canadian Medical Association Journal, found that the application of computer-aided detection (CADe) and computer-aided diagnosis or differentiation (CADx) to existing screening methods is paving the way for improved colorectal cancer diagnostics and patient care.

“In recent years, there has been a rapid expansion of research into the use of AI in gastroenterology, in particular for the detection of colorectal cancer,” notes Byrne. “Already, several studies have shown that AI can significantly improve cancer detection, which has further fueled research interest in this area.”
“The lifetime risk of developing colorectal cancer is around five to six per cent, making it a leading cause of cancer.”
Colorectal cancer is defined as a tumour of the rectum or colon, which is also called the large intestine. Biannual colorectal cancer screening using the fecal immunochemical test is recommended for individuals aged 50 to 74 years. For individuals with a family history of colorectal cancer or a personal history of adenomas — non-cancerous tumours — a colonoscopy is recommended every five years.
“We know that for every one per cent increase in early cancer detection, the risk of mortality from colorectal cancer decreases threefold.”
During a colonoscopy, a physician inserts a thin tube-shaped instrument called an endoscope into a patient’s rectum. The endoscope is equipped with a camera lens and white light to examine tissues and structures within the rectum and colon. Specialized endoscopes can also be used to remove suspicious polyps.
“The current practice is to remove all polyps seen in the colonoscopy examination and send the tissue to the pathology laboratory for analysis,” says Byrne. “It can take several days to receive the test results at the clinician’s office and book a follow-up appointment with the patient, as opposed to being able to diagnose and treat in one visit using CADe and CADx.”
Giving patients real-time results with computer-aided colonoscopy
CADe is a computer algorithm that uses machine learning to scan for and detect possible lesions in the colon in tandem with white light and camera colonoscopy.
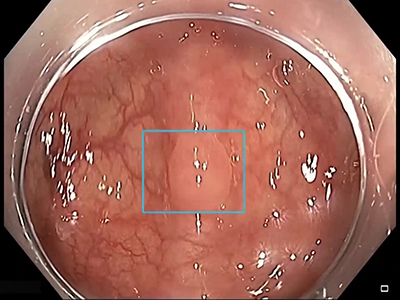
CADx characterizes detected lesions by performing real-time optical biopsies, circumventing the need to wait for lab results.
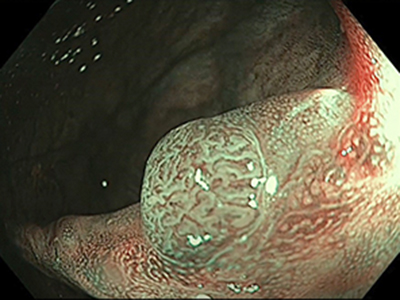
High-magnification and blue/green light allows CADx to zero in on abnormal pigments frequently found in colorectal polyps and tumours. CADx operators can then make an instant diagnosis of abnormal tissue. Based on its morphology, a clinician may decide to leave the abnormal tissue in place; excise it and discard it; or remove it, keep it and send it to a lab.
“Lesions less than five millimetres in size are almost always benign,” notes Byrne. “In many cases, it is possible to leave these in place or resect and discard them without sending them to a lab for analysis.”
Several research groups have shown that CADx biopsy results can equate to or exceed the precision of white light and video endoscopy alone in identifying suspect tissue, notes Byrne.
“Computer-aided polyp and tumour detection could improve the overall detection of precancerous lesions during colonscopy, which could ultimately save lives.”
“Clinicians can miss things, including small and large polyps,” says Byrne. “CADe can help detect lesions that the physician did not see or has already seen. CADx allows them to conduct live pathology evaluations that can involve removing suspect tissue during the examination — saving the patient time and possibly anxiety that come with having to book a follow-up appointment.”
“Patients who receive CADx may well leave the examination room much more reassured.”