Technological advances show promise as an extra oversight for the work of radiologists and pathologists.
New developments in the area of artificial intelligence (AI) are setting the stage for a digital brain to complement medical minds. Like the transition from rotary phones to smartphones, advances in AI technology are set to revolutionize how researchers and clinicians share and analyze information. This could have huge implications for the estimated 22,900 Canadian men who will be diagnosed with prostate cancer in 20191.
“AI could improve the efficiency and accuracy of diagnostic procedures, decreasing costs and getting patients’ test results back faster,” says Dr. Larry Goldenberg, a Vancouver Coastal Health Research Institute scientist and a founding director of the Vancouver Prostate Centre.
“AI could potentially help with making decisions on the best course of action to treat disease.”
Developed in the 1950s, AI simulates human intelligence, but with superhuman information processing abilities. Machine learning is a branch of AI that uses computer algorithms, or mathematical models, to predict outcomes.
Goldenberg’s recent article on AI and machine learning in prostate cancer, published in Nature Reviews, outlines several potential applications and outcomes of AI technology on prostate cancer research and care.

In particular, Goldenberg notes that AI shows promise as an extra check and balance for the work of radiologists and pathologists.
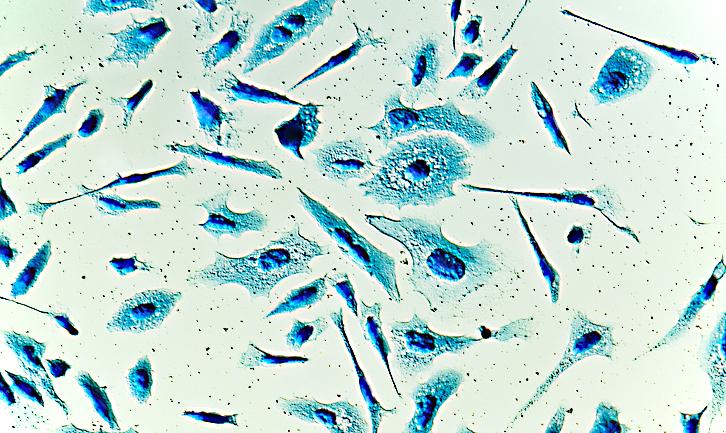
In pathology, clinicians currently look at slides of tissue samples under microscopes. For machine learning algorithms, clinicians scan and upload very high-resolution digital images of tissue samples—with patient information removed—to the software, which can then sift through thousands of images in the blink of an eye.
“A computer can have access to billions of pieces of information and, drawing from that, be able to see disease attributes humans cannot.”
Each digital slide is painstakingly labeled to teach the software how to identify samples of different diseases, as well as disease-free tissues. The software then uses information from its training to make predictions about disease types that may be present, and their level of severity.
“If we train computers to identify the likely outcome of a disease like prostate cancer based on images of similar prostate cancers, patients and clinicians will be in a better position to decide between waiting and seeing how the cancer may progress or opting for more invasive treatment, such as surgery or radiation,” explains Goldenberg.
For example, intermediate-risk prostate cancers can behave in a benign or aggressive way. Looking at a tissue sample of prostate cancer under a microscope does not typically reveal how it will behave. However, machine learning could analyze the scanned images for features that represent the genes of cells present in the cancer, and compare that to examples of similar cancers and their known outcomes. It could then use that information to predict whether the cancer is more likely to be aggressive or non-aggressive, and whether the patient should undergo surgery right away.
“The holy grail will be for AI to see things that the human eye does not see, and help us with more precise diagnoses and treatments.”
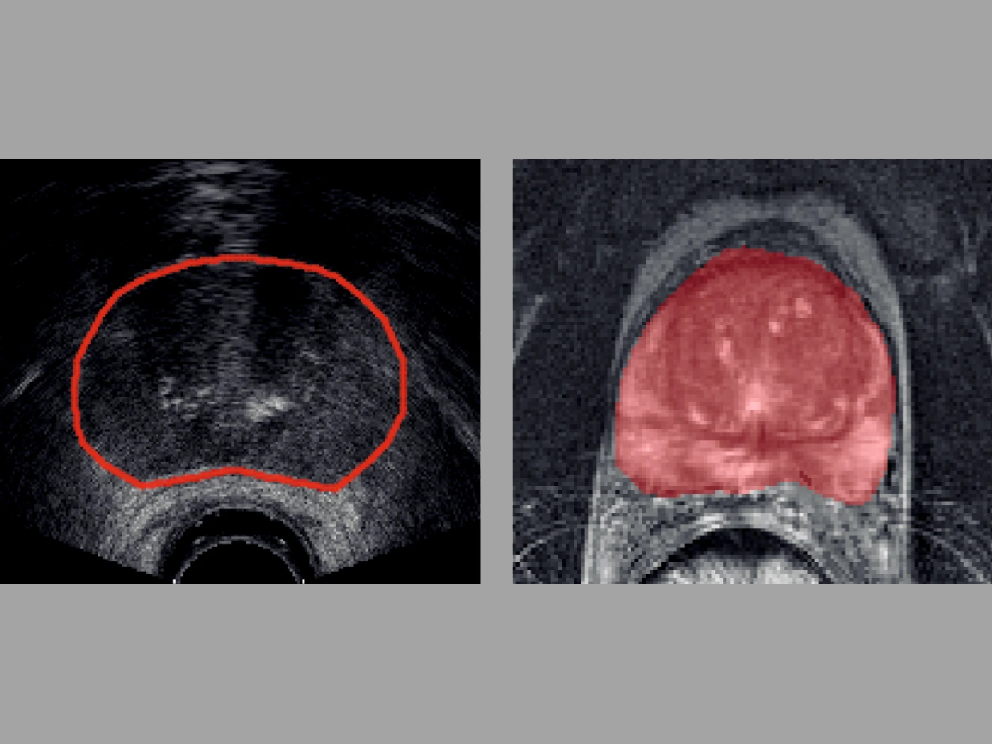
The added bonus of using the superhuman power of a computer is that it could enhance patient-specific targeted care, says Goldenberg. Digitized data—from slides of tissue samples to CT and MR scans—from different departments and areas of specialization could also be integrated into one centralized system, giving clinicians access to almost limitless clinical data for use in personalized medicine.
Future applications of AI in clinical care
AI is currently used in a limited capacity to make predictions about injuries and the presence of disease found in MRI and CT scans. However, its application is also being investigated for spinal cord injuries, ovarian cancer, pathology, prostate cancer and other areas of research and care.
Apart from diagnostics, AI is also being looked at to help guide surgeries, such as radical prostatectomies—where the prostate gland and some surrounding tissues are removed. AI-driven robotic aids can take over repetitive tasks, such as repositioning cameras used during laparoscopic surgery.
Source: Nature Research
In the future, AI could help meet growing health care needs by providing quality assurance and second opinions.
“The physician experts and tools that we have today are excellent,” says Goldenberg, “but if we can integrate machine learning into the clinic, we may be able to support the current work of clinicians and increase the accuracy and efficiency of medical processes and procedures.”


