
Several research teams are investigating new genome sequencing research headquartered in Vancouver to supercharge the discovery of tailored treatments.
Researchers at the Vancouver Prostate Centre are leading a multi-site clinical trial to explore new precision treatments for patients with prostate cancer. The Genomic-biomarker-selected Umbrella Neoadjuvant Study (GUNS) trial led by Vancouver Coastal Health Research Institute (VCHRI) researchers Dr. Lucia Nappi and principal investigator Dr. Martin Gleave will use genomic markers from study participant samples to make treatment recommendations for patients.
“We are incredibly excited about the potential for GUNS to enhance patient outcomes through a deeper understanding of prostate cancer drivers and treatment effectiveness,” states Gleave. “While our initial focus is on DNA and RNA sequencing, we anticipate that additional branches of this research will be introduced as novel discoveries to enhance patient care are made.”

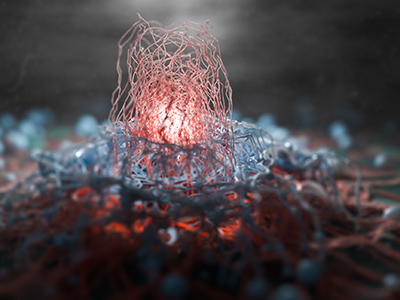
An evolving area of research, precision medicine is focused on personalizing treatments by using genomic and molecular profiling to identify unique gene changes in individuals and cancer tumours. Clinicians draw from published research, such as the anticipated peer-reviewed publications from the GUNS clinical trial, to help select the most promising therapy for disease suppression or eradication and to support patient recovery.
Both DNA and RNA are found in every living cell. DNA is the microscopic double helix composed of two chains of the bonded molecules adenine, guanine, cytosine and thymine. RNA mainly acts as a messenger between DNA and the creation of proteins.
“Currently, very few data sets on prostate cancer pathology include both DNA and RNA sequencing analysis,” says Nappi. Seeing prostate cancer cells at the genomic level gives researchers a fine-grained view of the inner-workings of the disease.
“The molecular profiling used in this study to view prostate cancer cells is similar to the image detail you can see on a high-definition television screen, compared to a regular television screen.”
Tailoring care at the genomic level
GUNS participants all have high- or very high-risk prostate cancer localized to the prostate only. All patients are screened at the outset of the trial based on a biopsy of their prostate cancer.
For the first eight weeks of the study, participants receive blood tests and androgen deprivation therapy — androgens are hormones that promote prostate cancer growth. Following the sequencing of their DNA, participants will be allocated to one out of four treatment streams.
“For example, if a participant’s prostate cancer has a genomic profile suggesting high dependence on the androgen receptor pathway, we will place them in the treatment stream designed to maximize their androgen inhibitor therapy,” notes Nappi. “This treatment involves two oral medications and one injection medication that targets the same androgen receptor pathway.”
“On the other hand, if we find genes in a participant’s prostate cancer that are associated with a poorer response to hormone therapy, or a more aggressive form of prostate cancer, we will place the participant in the stream that receives hormone therapy in combination with either immunotherapy or chemotherapy.”

At the conclusion of the trial, participants will receive a radical prostatectomy — the removal of the prostate gland and surrounding lymph nodes.
“The DNA and RNA analysis of the whole excised prostate after the trial will help us see how the treatment streams affected each patient’s prostate cancer, providing an extra layer of detail to our investigation.”
“The tumour samples taken before and after the trial will give us a more detailed and bigger picture view of: why treatments may or may not have worked, molecular pathways that could lead to treatment resistance and possible opportunities to enhance treatment effectiveness,” says Nappi.
In the coming years, the GUNS research study is expected to extend into the United States, with the potential for global expansion.


